A chain is only as strong as its weakest link: Using a “cascade of care” approach to evaluate gaps in the opioid use disorder treatment pipeline
There are persistent gaps in the addiction “science-to-practice” pipeline that lead to marked differences in treatment availability and quality. A cascade of care is one way of assessing where gaps in the provision of empirically supported addiction care exist. Despite increased funding and policy support to address harms, opioid overdose rates remain high. Therefore, it is critical to understand at which points the health care system is failing to provide appropriate care for people with opioid use disorder (OUD) and to assess disparities in receipt of medication for OUD. The current study sought to address this by using a cascade of care model to assess treatment quality and outcomes for OUD in the Florida Medicaid population.
WHAT PROBLEM DOES THIS STUDY ADDRESS?
Medications such as buprenorphine (often prescribed in formulation with naloxone and known by the brand name Suboxone) and extended-release naltrexone (often referred to by the brand name Vivitrol) are first-line treatments for OUD. The positive effects of these medications on short-term outcomes (e.g., reduced overdose, decreased opioid use and increased opioid abstinence, and withdrawal symptom relief) are well documented. Despite the availability of these lifesaving medications, long-term opioid abstinence rates remain low and overdose deaths remain high. This juxtaposition highlights the need to assess where gaps in the provision of effective addiction care exist. Continuous coverage, adequate provider capacity, ease of access in terms of location and time, treatment that addresses patient needs, preferences, and abilities to pay for, obtain, and use medications on schedule, and ongoing efforts to support treatment adherence are all necessary to provide care that improves health. A cascade of care is one way of assessing where gaps or drops in the provision of effective care exist. A cascade of care begins with the population prevalence, then calculates the number/percent of the population who are identified or diagnosed as having a condition, the number/percent who begin treatment, the number/percent who continue in or complete treatment and the number/percent who have positive treatment outcomes. Cascades of care can help system planners to better understand where there are system failures and develop targets for improvement. In this study, authors applied the cascade of care approach using administrative claims data to evaluate the quality of care for individuals with OUD in a single US state, Florida.
Figure 1.
HOW WAS THIS STUDY CONDUCTED?
This study applied a cascade of care model to data from two publicly available sources in order evaluate treatment quality and treatment outcomes for OUD in the state of Florida. Prevalence was established using the National Survey on Drug Use and Health (NSDUH) from 2016–2017 restricted data set online query tool applied to Florida. Data from Florida Medicaid claims for 2017 and 2018 were used to calculate the number of enrollees who were diagnosed with OUD, began medication for OUD, were retained on medication for a minimum of 180 days, and who died. Death dates through 12/31/18 were collected from the Medicaid enrollment database and matched to the study population. They also examined the location of diagnosis and the type of diagnosis (primary versus secondary) for differences. A primary diagnosis implies a patient seeking or being offered treatment for OUD. A secondary diagnosis implies treatment for some other condition as primary, but OUD being a significant contributor or important enough to note in a medical claim file. They went on to examine if there were observable differences in treatment receipt by age, sex, and race/ethnicity.
WHAT DID THIS STUDY FIND?
Roughly 2% of Florida Medicaid recipients were diagnosed with opioid use disorder and only 28% of those diagnosed with opioid use disorder began treatment with an FDA approved medication for opioid use disorder.
Prevalence of OUD for Florida Medicaid recipients from the NSDUH 2017 data 1.83% or approximately 28,370 persons. In 2017, Florida Medicaid enrollees who had an OUD had a high probability of having been diagnosed. However, only 28% of those diagnosed with OUD went on to be treated with an FDA approved medication for their OUD.

Figure 2.
Those that remained on a medication to treat opioid use disorder for at least 180 days were 5 times less likely to die.
Once on medication, 38% of newly diagnosed enrollees were retained in treatment for 180 days. Those who remained on medication for OUD for 180 days had a 2% chance of dying, whereas those that did not had a 10% chance.
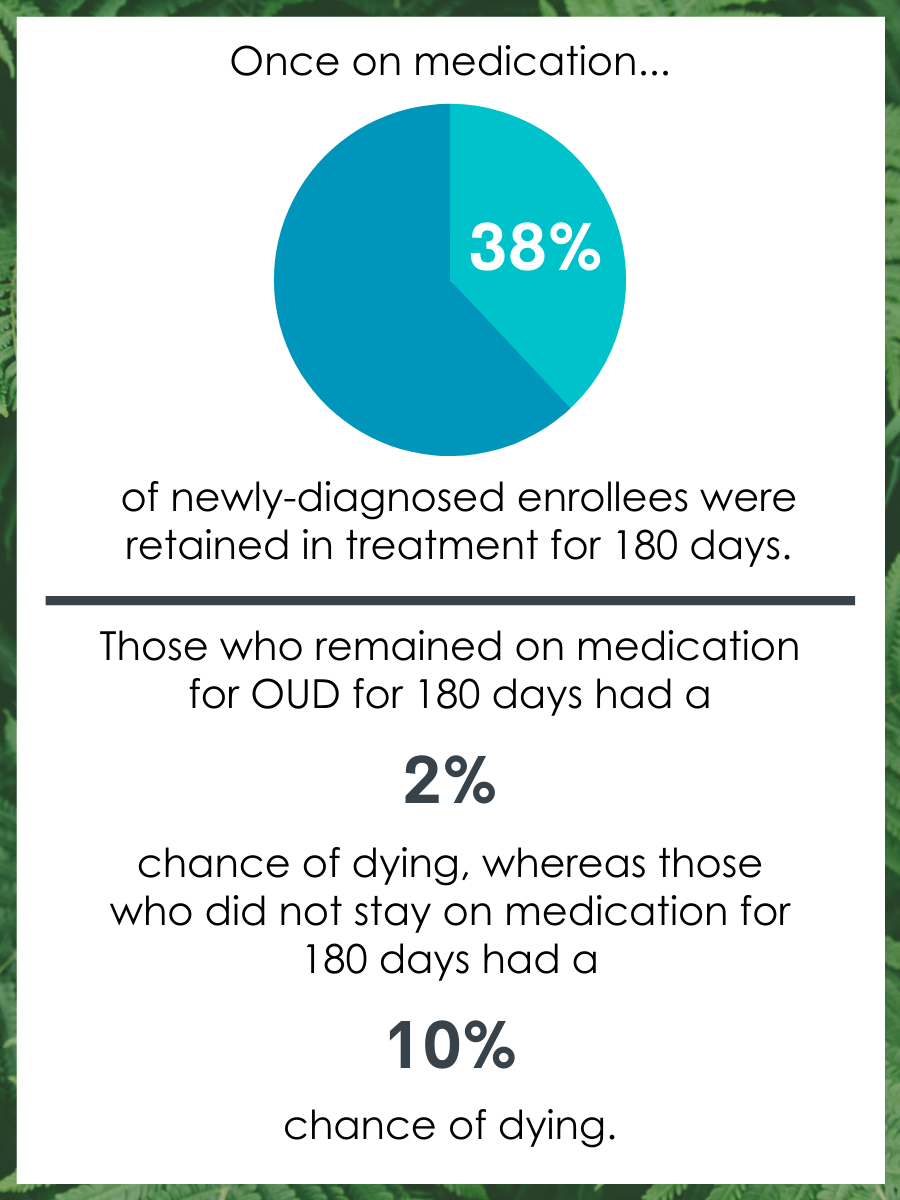
Figure 3.
Receiving a secondary diagnosis of opioid use disorder was associated with only a 2% chance of being treated with a medication for opioid use disorder.
57% of individuals diagnosed with OUD in 2017 received it as a secondary diagnosis and 90% of secondary diagnoses made were in hospital or physician-office settings. Of these only 2% received any medication for OUD.
People over age 50 and those that identified as Black were less likely to receive a primary diagnosis and consequently were less likely to receive medication for opioid use disorder.
People over age 50 and those that identified as Black were less likely to receive a primary diagnosis and consequently were less likely to receive treatment for OUD. People who were dually eligible for Medicaid and Medicare are also less likely than people who are Medicaid eligible only to receive a primary diagnosis of OUD.
WHAT ARE THE IMPLICATIONS OF THE STUDY FINDINGS?
This study found a few interesting gaps in the OUD treatment pipeline. First, only 28% of those diagnosed with OUD began treatment with an FDA approved medication for OUD (primarily methadone or buprenorphine and a small number naltrexone). Second, remaining on a medication to treat OUD for at least 180 days was associated with a five-fold reduced risk of death. This is consistent with previous research demonstrating reduced overdose risk associated with agonists is only present when individuals remained on the agonist for at least 180 days. Third, receiving a diagnosis at a medical facility was associated with only a 2% chance of receiving a medication for OUD. And finally, that those over age 50 and those that identified as Black were less likely to receive a primary diagnosis and consequently were less likely to receive treatment for OUD despite similar prevalence rates. These findings highlight how using a cascade of care approach to evaluate claims data for OUD was feasible and informative. The findings provide critical insights for administrators and policymakers. The authors were able to identify key differences in treatment utilization based on where a diagnosis was made and linked poor treatment retention to increased odds of death. Policymakers can use a cascade of care as for systems planning, resource allocation, and quality improvement activities.
The issues raised in this analysis are important for planning purposes in Florida and should be both replicated and examined in other states. They identified subpopulations who are less likely to receive treatment including people over age 50, people who are Black, and those who are dually Medicaid and Medicare eligible. This study points to a need for better coordination and continuity of care between general medical settings (physician offices, hospitals, ED), where OUD medication receipt was less likely, and specialty care providers. An OUD diagnosis, regardless of whether it is primary or secondary or who makes the diagnosis requires treatment. To leave these patients untreated is major gap in the current system that is associated with the worst possible outcome – death. It is important to note, OUD like all SUD diagnoses is incredibly heterogeneous and to aid practitioners with selecting treatment options there are mild/moderate/severe impairment markers. It is possible, though speculative, that OUD as a secondary diagnosis may indicate prescription misuse or less severe OUD and that’s why medications were not recommended.
- LIMITATIONS
-
- Prevalence estimates were based on a national household survey. This means that individuals that were currently incarcerated, housing insecure, or living in a shelter/institution were likely systematically excluded.
- Florida Medicaid population is not representative of other states nor the larger population of individuals with OUD national and internationally.
- It is unclear why those with OUD did not receive medication whether primary or secondary.
- This analysis did not have a way to appropriately account for loss of coverage during the year under investigation.
- Cause of death was not available in the data. Thus, it is not clear if OUD was directly linked to death despite being associated with differences in death rates.
BOTTOM LINE
- For individuals and families seeking recovery: This study found a few potentially critical gaps in the OUD treatment pipeline. First, only 28% of those diagnosed with OUD began treatment with an FDA approved medication for OUD. Second, remaining on a medication to treat OUD for at least 180 days was associated with a five-fold reduced risk of death. Third, receiving a diagnosis at a medical facility was associated with only a 2% change of received a medication for OUD. And finally, that those over age 50 and those that identified as Black were less likely to receive a primary diagnosis and consequently were less likely to receive treatment for OUD. For individuals in recovery, findings here are in line with other studies that highlight the lifesaving benefits of being treated with a medication for OUD and, that if you are being treated with medication, remaining on it for at least 180 days may be the best approach to ensure success. It also highlights that individuals who are diagnosed in a medical setting, and who are older than 50, and/or identify as Black are much less likely to receive this live saving treatment and may need to advocate for them, if not offered. The exact reason for this is unclear and further research is needed
- For treatment professionals and treatment systems: This study found a few interested gaps in the OUD treatment pipeline. First, only 28% of those diagnosed with OUD began treatment with an FDA approved medication for OUD. Second, remaining on a medication to treat OUD for at least 180 days was associated with a five-fold reduced risk of death. Third, receiving a diagnosis at a medical facility was associated with only a 2% change of received a medication for OUD. And finally, that those over age 50 and those that identified as Black were less likely to receive a primary diagnosis and consequently were less likely to receive treatment for OUD despite similar prevalence rates. Taken together, this study highlights a few ways in which the system is not working for many that need it. Thus, those that work in these systems may need to diagnose weak links in the cascade of care provided to understand the reasons for these deviations from best practices. It may also mean advocating for system changes necessary to ensure those that need services do not fall through the cracks. Specifically, that all those that qualify should be offered medication to treat their OUD and have a system that permits at least a 180-day course of medication. Additionally, creation of checks that ensures equitable prescribing will help many that were systematically not prescribed medications.
- For scientists: This study found a few interesting gaps in the OUD treatment pipeline. First, only 28% of those diagnosed with OUD began treatment with an FDA approved medication for OUD. Second, remaining on a medication to treat OUD for at least 180 days was associated with a five-fold reduced risk of death. Third, receiving a diagnosis at a medical facility was associated with only a 2% change of received a medication for OUD. And finally, that those over age 50 and those that identified as Black were less likely to receive a primary diagnosis and consequently were less likely to receive treatment for OUD despite similar prevalence rates. The takeaway from this study for scientist is that there is still a lot of work to do to diagnose weak links in the cascade of care provided to understand the reasons for deviations from best practices and ultimately to patch up a leaky science to practice pipeline. Increased work in implementation science has potential to address these areas. Also, investigation into why particular sub-groups of patients such as those that over 50 and/or identified as Black were less likely to received medication, is warranted.
- For policy makers: This study found a few interested gaps in the OUD treatment pipeline. First, only 28% of those diagnosed with OUD began treatment with an FDA approved medication for OUD. Second, remaining on a medication to treat OUD for at least 180 days was associated with a five-fold reduced risk of death Third, receiving a diagnosis at a medical facility was associated with only a 2% change of received a medication for OUD. And finally, that those over age 50 and those that identified as Black were less likely to receive a primary diagnosis and consequently were less likely to receive treatment for OUD despite similar prevalence rates. Policymakers can use a cascade of care as part of an overall approach to help with systems planning, resource allocation, and quality improvement activities.
CITATIONS
Johnson, K., Hills, H., Ma, J., Brown, C. H., & McGovern, M. (2020). Treatment for opioid use disorder in the Florida Medicaid population: Using a cascade of care model to evaluate quality. The American Journal of Drug and Alcohol Abuse, [Epub ahead of print]. doi: 10.1080/00952990.2020.1824236
